Vitamin D is a fat-soluble vitamin that helps in the absorption of calcium and phosphate to the body and hence very important for healthy bone, teeth & muscles. Deficiency of vit-D can hence cause bone deformities among children and bone pain (osteomalacia) among adults.
There are 2 major types of Vitamin D – Vitamin D2 (Ergocalciferol) & Vitamin D3 (Cholecalciferol).
VitD2 is seen in plant-based products such as mushrooms, while VitD3 is seen in animal products such as liver, egg, fatty fish, etc. Our body (skin) can also produce Vit-D3 by itself, from cholesterol, when exposed to sunlight (ultraviolet B radiation).
Vitamin D3 is more effective at improving Vitamin D Status and hence most of the dietary supplements and Vitamin D tablets contain Cholecalciferol. It is also seen along with most of the Calcium supplements to facilitate the absorption of calcium into the body. Excess of vitamin D can, however, create excess calcium deposits (hypercalcemia) and kidney diseases
Low Vitamin D – A Common Condition
Low vitamin D is prevalent among Indians due to a combination of lifestyle, dietary habits, and environmental factors. One primary reason is the limited exposure to sunlight, which is a natural source of vitamin D. Many people in India, especially those with indoor jobs, may not get enough sunlight, leading to insufficient vitamin D synthesis in the skin. Additionally, cultural practices like covering the body with clothing for modesty or religious reasons further reduce skin exposure to sunlight.
Dietary patterns also contribute to low vitamin D levels in the Indian population. Traditional diets may lack sufficient vitamin D-rich foods, and there might be limited awareness about the importance of including such foods in daily meals. These factors collectively contribute to the widespread prevalence of low vitamin D levels, emphasizing the need for awareness campaigns, dietary adjustments, and, when necessary, supplementation to address this common nutritional deficiency.
In addition to limited sunlight exposure and dietary factors, the prevalence of low vitamin D levels among Indians is influenced by the presence of melanin in the skin. Melanin, the pigment responsible for skin color, acts as a natural sunscreen and reduces the skin’s ability to produce vitamin D in response to sunlight. This means that individuals with darker skin tones may require more extended sun exposure to meet their vitamin D needs compared to those with lighter skin.
Furthermore, the problem is exacerbated in densely populated and polluted urban areas. The high levels of air pollution in cities can hinder the penetration of ultraviolet B (UVB) rays, essential for vitamin D synthesis, through the atmosphere. As a result, even individuals spending time outdoors may not receive adequate UVB exposure, contributing to the widespread prevalence of low vitamin D levels, particularly in urban populations. Addressing these multifaceted factors is crucial in developing effective strategies to combat vitamin D deficiency in the Indian context
How is Vit-D formed in the body?
Vitamin D is primarily synthesized in the body through a process that involves the skin, sunlight, and subsequent metabolic reactions. Here’s a brief overview:
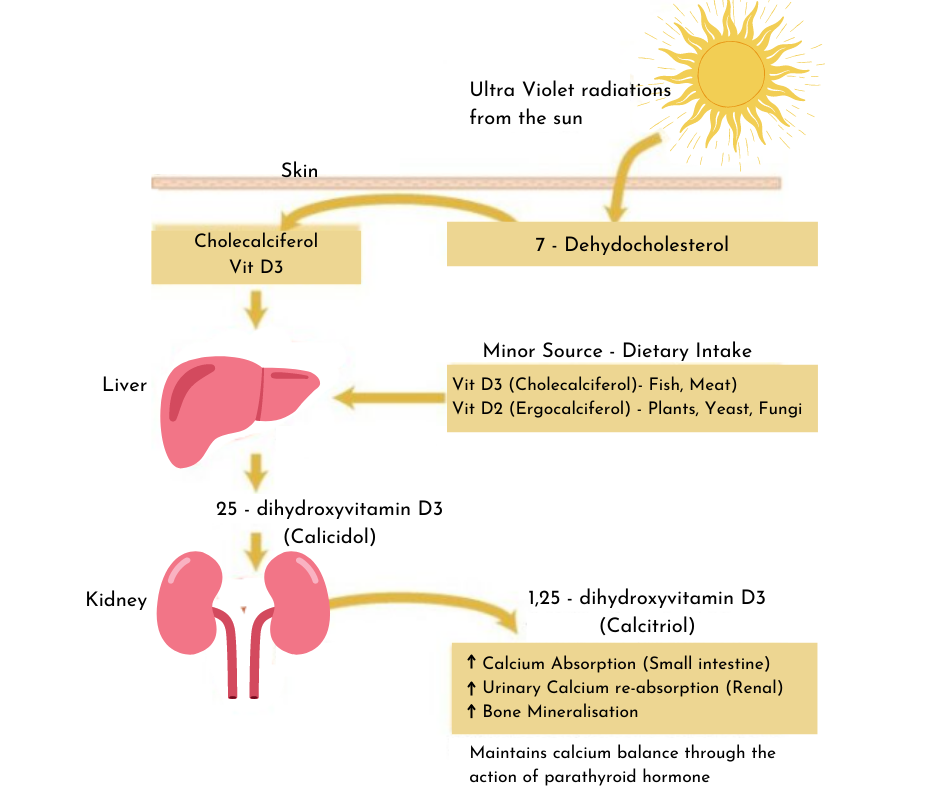
- UVB Exposure: The first step in vitamin D synthesis occurs when the skin is exposed to ultraviolet B (UVB) radiation from sunlight. UVB rays penetrate the skin and react with 7-dehydrocholesterol, a compound present in the skin cells.
- Formation of Pre-Vitamin D3: The interaction between UVB rays and 7-dehydrocholesterol triggers a chemical transformation, converting 7-dehydrocholesterol into previtamin D3. This pre-vitamin D3 is not yet active as vitamin D.
- Conversion to Vitamin D3: Heat from the sun or body temperature facilitates the conversion of previtamin D3 into vitamin D3 (cholecalciferol). This conversion is a crucial step in making vitamin D biologically active.
- Liver Metabolism: Vitamin D3 is then transported to the liver through the bloodstream. In the liver, it undergoes further metabolic changes, turning into calcidiol or 25-hydroxyvitamin D.
- Kidney Activation: The final activation step occurs in the kidneys, where calcidiol is converted into the active form of vitamin D known as calcitriol or 1,25-dihydroxyvitamin D. This activated form plays a crucial role in regulating calcium and phosphorus metabolism in the body.
This entire process illustrates how exposure to sunlight, particularly UVB rays, initiates the synthesis of vitamin D in the skin, which is then further metabolized in the liver and kidneys to become biologically active and functional in various physiological processes.
How to overcome low Vit-D levels?
- Sun Exposure: Aim for moderate sun exposure, preferably in the early morning or late afternoon when the sun is less intense. Spend around 15-30 minutes outdoors, ensuring that a significant portion of your skin is exposed.
- Dietary Changes: Include vitamin D-rich foods in your diet such as fatty fish (like salmon and mackerel), fortified dairy products, eggs, and mushrooms. Consider consulting with a nutritionist to create a meal plan that boosts your vitamin D intake.
- Supplementation: Periodically taking vitamin D supplements, especially during seasons or in regions where sunlight exposure is limited, can be beneficial. Consult with a healthcare professional to determine the appropriate dosage based on your individual needs and health status.
- Regular Health Check-ups: Schedule regular health check-ups to monitor your vitamin D levels. This allows for timely adjustments in your sun exposure, dietary habits, or supplementation plan based on your body’s specific requirements.
- Optimize Sun Exposure: Choose outdoor activities that allow for sun exposure, such as walking, jogging, or gardening. However, be mindful of sunscreen use, as it can inhibit vitamin D synthesis. Balance sun safety with adequate exposure.
While sunlight is essential for vitamin D synthesis, it’s crucial to strike a balance in sun exposure. Overexposure without adequate protection can lead to skin damage and increase the risk of skin cancer. Being sensible about sun exposure, using sunscreen, and seeking shade when necessary ensures the benefits of vitamin D synthesis while prioritizing skin health
Also Read: Cancer – Lifestyle Strategies for Prevention
Risk of over-supplementation
While addressing vitamin D deficiency through supplementation is crucial, it’s equally important to be aware of the potential risks associated with over-supplementation. Excessive intake of vitamin D, usually through high-dose supplements, can lead to a condition called hypervitaminosis D. This condition may result in elevated levels of calcium in the blood (hypercalcemia), which can manifest in symptoms such as nausea, vomiting, weakness, and even more severe complications like kidney damage. Hypervitaminosis D, resulting from high vitamin D levels, may disrupt the balance of calcium in the body. This imbalance can affect the electrical signals in the heart, potentially leading to irregular heart rhythms or arrhythmias. It’s essential to strictly adhere to recommended dosage guidelines provided by healthcare professionals and not self-prescribe high doses without proper guidance.
Moreover, prolonged and excessive vitamin D supplementation may negatively impact other aspects of health. While vitamin D plays a crucial role in calcium absorption and bone health, an imbalance caused by excessive supplementation may lead to the calcification of soft tissues, including blood vessels and kidneys. This emphasizes the importance of moderation and individualized guidance when considering vitamin D supplementation. Regular monitoring of vitamin D levels through healthcare professionals can help ensure that supplementation remains within safe and beneficial limits for overall health.


This Post Has One Comment
Pingback: NuvoVivo: A Comprehensive Journey to Health and Vitality - NuvoVivo: Reverse Your Age & Lifestyle Diseases